Atopic dermatitis
Atopic dermatitis
Pathophysiology
Atopic dermatitis is the most common type of eczema that affects millions of people worldwide.
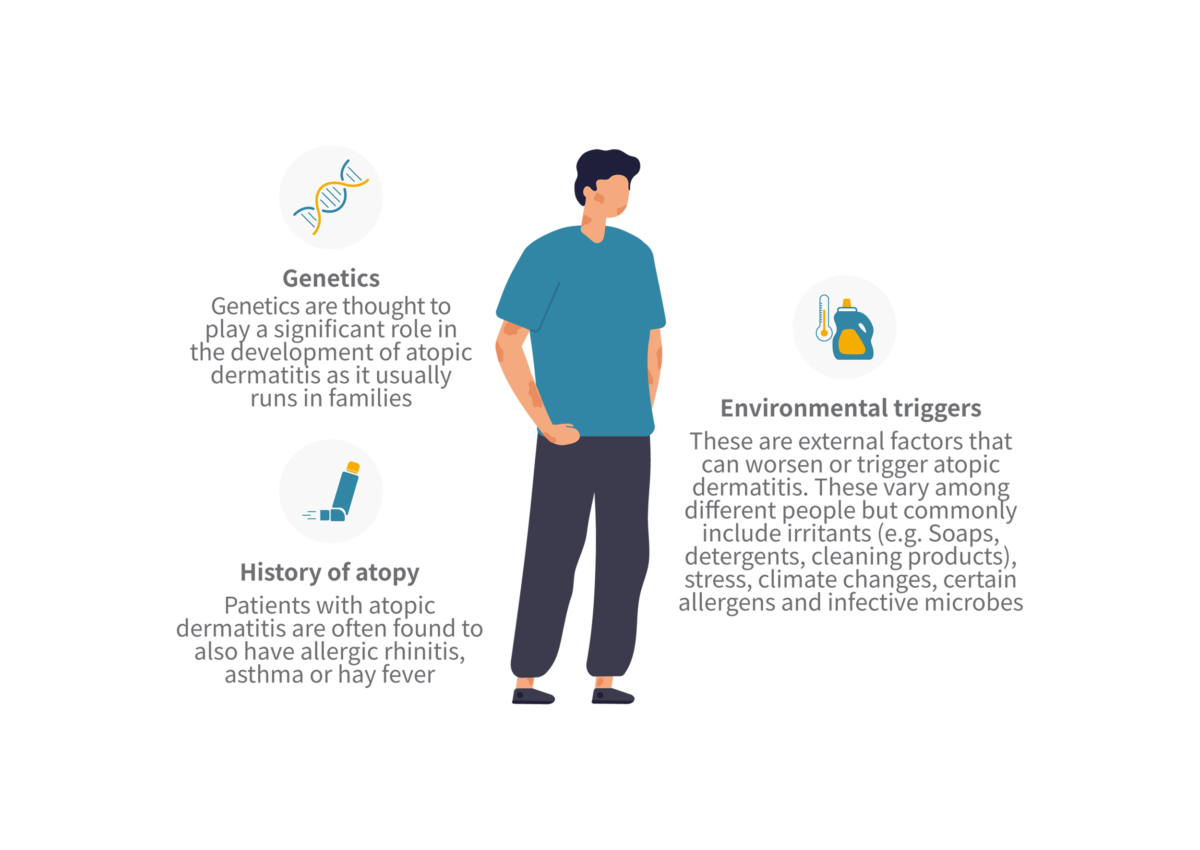
Major risk factors
1. Genetics: Genetics are thought to play a significant role in the development of atopic dermatitis as it usually runs in families.
2. Environmental triggers: These are external factors that can worsen or trigger atopic dermatitis. These vary among different people but commonly include irritants (e.g., soaps, detergents, cleaning products), stress, climate changes, certain allergens and infective microbes.
3. History of atopy: Patients with atopic dermatitis are often found to also have allergic rhinitis, asthma or hay fever.
Symptoms
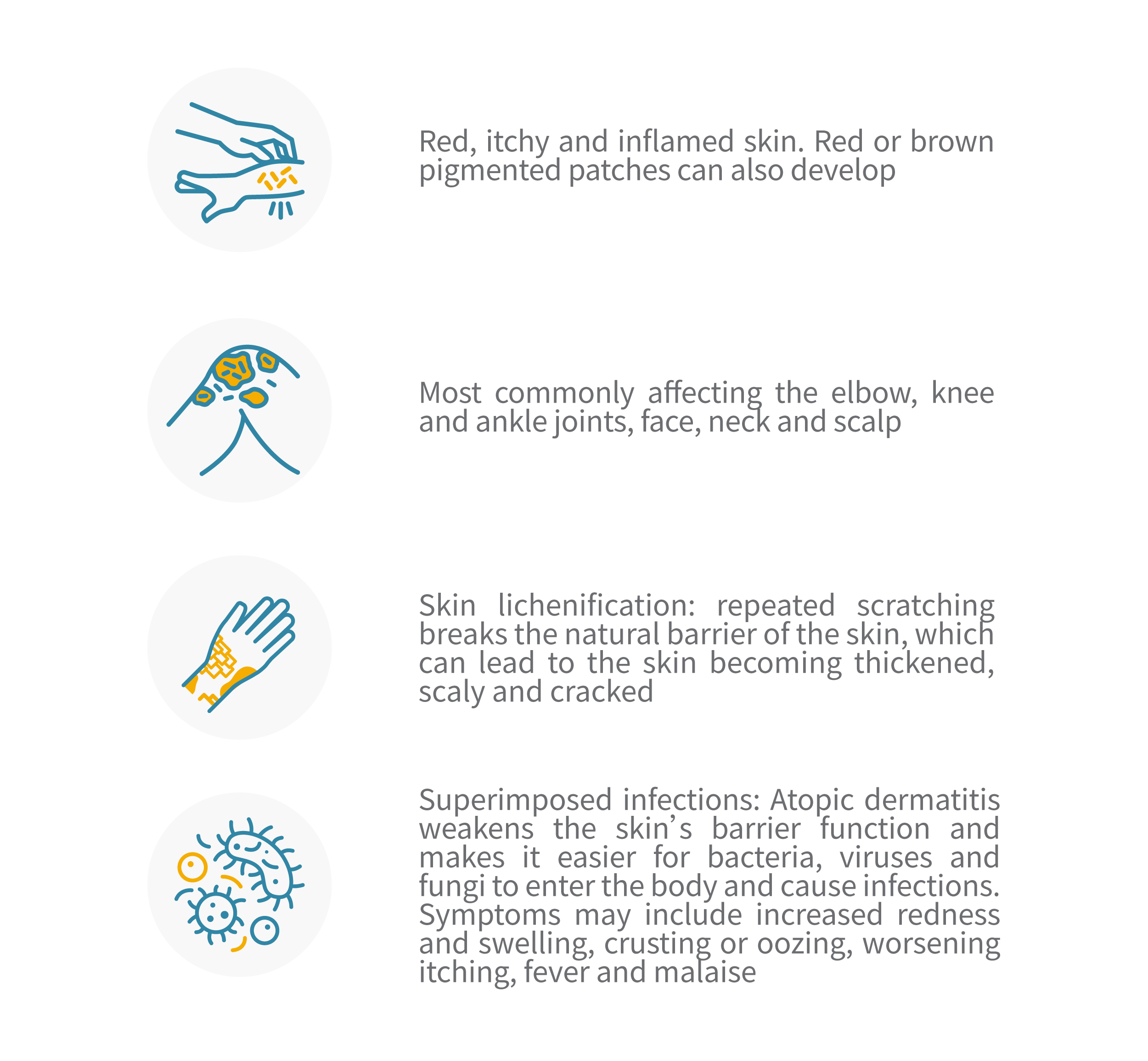
Common symptoms can include:
Effect
The burden of atopic dermatitis may affect the physical, emotional and social aspects of the patient’s life.
- Physical: Patients may experience symptoms such as itchiness, pain and oozing. In severe cases, this may require hospitalisation for treatment of superimposed infections or intensive, specialised care from nurses.
- Emotional: Atopic dermatitis can cause stress, anxiety and depression. Often, it may impact a patient’s self-esteem and body image.
- Social: Atopic dermatitis can lead to social isolation and discrimination. It may impact relationships, employment and other aspects of daily living.
Treatment
The goal of treatment is to achieve symptom improvement and long-term control. The specific treatment will depend on the severity of the disease and the individual symptoms and control.
- Topical corticosteroids: These are anti-inflammatory medications that can reduce redness, itching and inflammation. They are available in various strengths and formulations depending on your disease.
- Antibiotics: May be prescribed if there is a superimposed bacterial infection.
- Immunosuppressants: Typically used in moderate to severe cases that are not responsive to first-line topical treatments or steroids.
- Phototherapy (or light therapy)
- Biologics (injectables): In certain cases, biologics may be useful in the treatment of atopic dermatitis. Biologics work by targeting specific molecules in the immune system involved in the inflammatory process. These include anti-interleukin 4/13, such as dupilumab (Dupixent).
Recovery
Lifestyle modifications:
- Keep the skin moisturised: Regular use of moisturisers can offer a barrier for the skin and minimize further exacerbations.
- Avoid harsh soaps and detergents with strong perfumes or aromas.
- Take short, lukewarm baths or showers. Avoiding hot baths will reduce excessively drying the skin.
- Wear loose-fitting, breathable clothings.
- Stress management: Good stress management can minimize eczema flares.

